The importance of data interoperability in healthcare is well-established, offering a plethora of benefits such as enhanced patient safety, improved quality of care, streamlined administrative processes, and simplified reporting. Initially driven by regulatory mandates, today, additional factors like data-driven decision-making and evolving patient expectations are fueling its adoption.
The regulatory landscape has continuously evolved since the introduction of the first set of Fast Healthcare Interoperability Resources (FHIR) in 2013. FHIR, developed by the standards body Health Level 7 (HL7), facilitates the exchange of Electronic Health Records (EHR). Notably, the Cures Act in the US, enacted in 2016, aims to expedite the discovery, development, and delivery of 21st-century cures, thereby emphasizing the importance of interoperability.
In May 2020, the Office of the National Coordinator for Health Information Technology (ONC) and the Department of Health and Human Services (HHS) issued the 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Final Rule. This rule aimed to enforce specific provisions of the Cures Act, including conditions and certification requirements for health IT developers under the ONC Health IT Certification Program. Additionally, it addressed the voluntary certification of health IT for pediatric healthcare providers and delineated activities deemed reasonable and necessary that do not constitute information blocking.
The implementation of these provisions sought to propel interoperability forward and bolster the access, exchange, and utilization of electronic health information. Furthermore, the rule solidified certain adjustments to the 2015 Edition Health IT certification criteria and program. These modifications were designed to promote interoperability, improve health IT certification, and alleviate burdens and costs within the healthcare ecosystem.
In June 2023, the HHS Office of Inspector General (OIG) issued the final rule to enforce penalties for information blocking as mandated by the Cures Act.
Following this, in December 2023, the ONC’s HTI-1 final rule was put into effect, incorporating critical provisions of the 21st Century Cures Act. This comprehensive rule not only updated the ONC Health IT Certification Program but also introduced new and enhanced standards, implementation specifications, and certification criteria. The HTI-1 final rule is designed to advance interoperability, transparency, and the efficient use of electronic health information.
Key aspects of the final rule include ensuring algorithm transparency, adopting United States Core Data for Interoperability (USCDI) Version 3 as a foundational standard, strengthening regulations against information blocking, and introducing new reporting metrics focused on interoperability for certified health IT systems. These measures are instrumental in driving forward interoperability efforts and emphasizing patient-centered care throughout the US healthcare system.
Amidst this rapidly evolving regulatory landscape, Healthcare Organizations (HCOs) are increasingly prioritizing interoperability. According to a Forrester report, 42% of “modern and future-fit HCOs” designate data interoperability and unlocking the value of data as a “critical priority.” While 33% of organizations focus on cost reduction, a higher percentage (40%) highlight improving customer experience as their top business objective, alongside revenue growth — a goal facilitated by interoperability.
Aonflow iPaaS – Free for First 3 Months!
Build and run up to 1,500 transactions monthly with no cost. No payment info needed!
Interoperability in Healthcare: Benefits and Opportunities
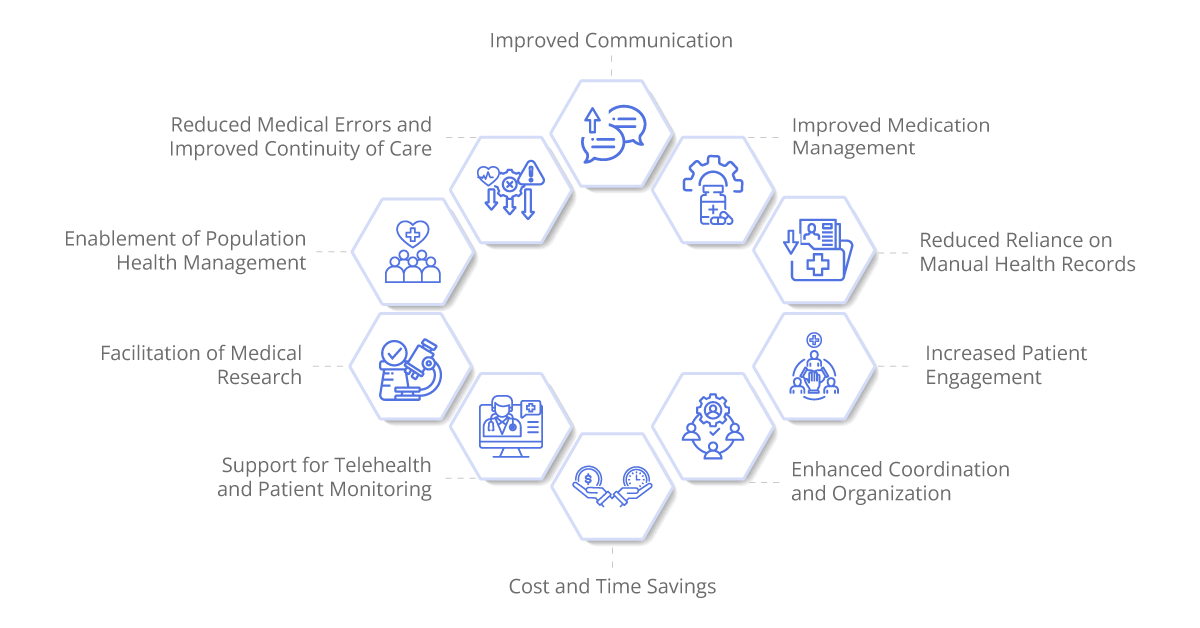
Interoperability stands as a cornerstone for Healthcare Organizations (HCOs), offering a multitude of benefits that significantly enhance patient care and operational efficiency:
Reduced Reliance on Manual Health Records: By facilitating seamless exchange of electronic health data, interoperability minimizes the need for manual health record management. This, in turn, mitigates the occurrence of duplicate health checks and ensures a more streamlined workflow.
Improved Medication Management: Interoperability enhances the accuracy, completeness, and timely access of patient data, thereby enabling healthcare providers to better manage medications. This leads to more informed decision-making, reduced medication errors, and ultimately, improved patient outcomes.
Cost and Time Savings: With interoperability, HCOs can reduce the time and resources traditionally required for treatment. By eliminating redundant tests, procedures, and paperwork, healthcare providers can optimize their workflow and allocate resources more efficiently.
Increased Patient Engagement: Interoperability empowers patients by providing them with greater access to their health information. This fosters active participation in their care journey, leading to improved patient satisfaction and adherence to treatment plans.
Enhanced Coordination and Organization: Interoperability enables seamless sharing of patient information across various healthcare settings and providers. This promotes better coordination of care, ensuring that all members of the care team have access to up-to-date patient data when making clinical decisions.
Reduced Medical Errors and Improved Continuity of Care: By facilitating the exchange of accurate and comprehensive patient information, interoperability helps reduce the occurrence of medical errors and ensures continuity of care across different healthcare settings and providers.
Improved Communication: Interoperability fosters better communication between healthcare professionals and patients. Access to timely and relevant health information enables more effective patient-provider communication, leading to improved patient satisfaction and outcomes.
Facilitation of Medical Research: Interoperability fuels medical research by providing researchers with access to large-scale healthcare data. This enables them to conduct studies and analyses that can lead to new insights, treatments, and advancements in healthcare.
Support for Telehealth and Patient Monitoring: Interoperability is essential for the success of telehealth and remote patient monitoring initiatives. It enables secure transmission of patient data between patients and healthcare providers, facilitating virtual consultations, remote monitoring, and telemedicine services.
Enablement of Population Health Management: Interoperability enables the aggregation and analysis of population health data. This provides HCOs with valuable insights into community health trends, enabling them to implement targeted interventions and population health programs that improve overall health outcomes.
Navigating Challenges in Healthcare Modernization and Interoperability
The drive towards healthcare interoperability is fueled by various factors such as the pursuit of efficient and cost-effective healthcare delivery, government initiatives, regulations aimed at enhancing patient care and safety, the advent of new medical technologies, and the widespread adoption of Electronic Health Records (EHRs). Despite these motivations, the road to implementation is fraught with challenges.
A significant hurdle in achieving interoperability is the persistence of outdated practices, with a staggering 70% of healthcare providers still relying on fax machines to exchange medical information. This reliance on antiquated communication methods not only impedes the seamless flow of data but also hampers the efficiency and effectiveness of healthcare delivery.
However, there is a growing recognition of the need for healthcare modernization, driven in part by initiatives such as those spearheaded by the Centers for Medicare and Medicaid Services (CMS). CMS has taken a proactive stance by advocating for the elimination of fax-based communication in US healthcare, signaling a pivotal shift towards embracing more advanced and interoperable technologies.
Embracing Composable Architecture for Agile Adaptation
A composable healthcare strategy enables organizations to leverage their existing IT infrastructure while seamlessly integrating newer capabilities in a modular fashion. This approach emphasizes interoperability, allowing different systems and applications to communicate and share data effectively. Gartner recommends the adoption of Interoperable Application Ecosystems (IAEs) as a practical means to achieve composable healthcare and orchestrate successful digital transformations.
Transitioning from Legacy Systems Using Hybrid Cloud Solutions
Despite the growing need for modernization, a 2021 Healthcare Information and Management Systems Society (HIMSS) survey revealed that a significant majority (73%) of healthcare providers still rely on legacy information systems. These outdated systems pose numerous challenges, including increased errors, slower processes, difficulties in adapting to modern healthcare demands, and gaps in compliance.
Healthcare organizations may upgrade their data management skills while preserving flexibility and scalability by fusing cloud technologies with on-premises infrastructure. Hybrid cloud solutions streamline the integration of new applications and programs, ensuring a continuous flow of data during system updates.
Enhancing Data Quality through Analytics, Audits, Metrics, and Standards
A 2020 study published in the JAMA Network revealed that 20% of patients discovered that there were errors in their Electronic Health Record (EHR) data. Additionally, a recent survey conducted by HIMSS and Patient ID unveiled that Healthcare Organizations (HCOs) dedicate an average of 109.6 hours per week to address patient identification issues, with over a third of organizations reporting annual expenditures exceeding US$1 million for identification resolution. Addressing these challenges necessitates a standardized approach to identity management. Improving healthcare data quality requires HCOs to implement comprehensive strategies that include auditing data management practices, adhering to industry-approved standards, integrating analytics, selecting relevant metrics, and providing ongoing staff training on data management solutions.
Government Funding and Pay-As-You-Go Models to Lower Costs
Transitioning from traditional workflows to interoperable healthcare systems entails substantial upfront costs. According to Global Market Insights, initial installation costs for software development and infrastructure in HCOs can surpass US$60,000 in the first year. To alleviate financial barriers, organizations should explore eligibility for government grants aimed at modernizing health record systems. Additionally, pay-as-you-go models offered by cloud vendors can help mitigate costs and enable long-term savings. Collaborating with a trusted IT services partner can facilitate the identification of affordable methods for modernization and utilization of cloud resources. This involves conducting thorough assessments of organizational workloads, identifying inefficiencies, conducting cost-benefit analyses, and developing phased plans for cloud adoption. Through strategic planning and leveraging available resources, HCOs can successfully navigate the transition to interoperable healthcare systems while managing costs effectively.
Leveraging Asset Tracking and APIs for Enhanced Cybersecurity
The security of patient data remains a paramount concern, highlighted by the alarming statistic that “more than 82.6 million healthcare records were exposed or impermissibly disclosed” in the US between January 1, 2023, and October 31, 2023, as reported by the HIPAA Journal. Health systems often underestimate the number of connected devices on their networks, according to insights from cybersecurity vendors outlined in a Forrester report. To address this critical challenge, Healthcare Organizations (HCOs) are increasingly turning to automation, particularly asset tracking, to accurately identify all connected devices and mitigate potential threats. By implementing robust asset tracking mechanisms, HCOs can enhance their cybersecurity posture and proactively safeguard patient data against unauthorized access and breaches.
Furthermore, streamlining and standardizing codes through Application Programming Interfaces (APIs) present an opportunity to bolster the efficiency and security of health data exchange. APIs enable seamless communication and data exchange between disparate systems, facilitating interoperability while adhering to stringent security protocols. By leveraging APIs, HCOs can optimize workflows, enhance data integrity, and strengthen cybersecurity measures, ultimately paving the way for process improvements and innovation in healthcare delivery.
Aonflow is the leading integration platform.
You can kick-start by integrating your first-ever workflow in just a matter of minutes.
Ensuring Compliance with Interoperability Standards
A significant challenge in advancing interoperability lies in the standardization of terminology and data normalization to align with evolving standards. Recognizing the critical importance of interoperability standards in digital health transformation, the World Health Organization (WHO) and Health Level 7 (HL7) have entered into a Project Collaboration Agreement to promote the global adoption of open interoperability standards. As interoperability standards continue to evolve at the local, national, and global levels, HCOs must remain vigilant and proactive in ensuring compliance. By adhering to interoperability standards, HCOs can foster seamless data exchange, promote care coordination, and unlock the full potential of digital health technologies to improve patient outcomes and enhance healthcare delivery worldwide.
Navigating Data Management Challenges in Healthcare
Managing unstructured data poses a significant obstacle to enhancing interoperability and delivering a connected care experience, as highlighted by approximately 50% of respondents from US hospitals and health systems in a Statista survey. To overcome these challenges, smart hospitals are leveraging innovative strategies to consolidate and standardize data, facilitating improved data generation and insights.
Addressing Silos and Consolidating Data
Smart hospitals recognize the importance of breaking down data silos and consolidating disparate data sources into a unified and standardized format. By centralizing data repositories and adopting interoperable systems, healthcare organizations can streamline data management processes and promote seamless data exchange across various departments and systems.
Unlocking Insights and Enhancing Decision-Making
Consolidating data into a standardized format enables healthcare organizations to unlock valuable insights and facilitate informed decision-making. By harnessing the power of advanced analytics and artificial intelligence, smart hospitals can derive actionable insights from vast amounts of data, leading to improved patient outcomes, operational efficiencies, and cost savings.
Embracing Innovation and Collaboration
Innovation and collaboration are essential components of overcoming data management challenges in healthcare. Smart hospitals leverage emerging technologies and collaborate with industry partners to develop robust data management solutions tailored to their specific needs. By staying abreast of technological advancements and fostering a culture of innovation, healthcare organizations can adapt to evolving data management requirements and drive continuous improvement in data governance and interoperability.
Harnessing iPaaS for Interoperability in Healthcare Systems
Integration Platform as a Service (iPaaS) is emerging as a pivotal tool for fostering interoperability within healthcare systems. As healthcare organizations strive to streamline operations and enhance patient care, iPaaS offers a robust solution for facilitating seamless data exchange and integration across disparate systems and applications.
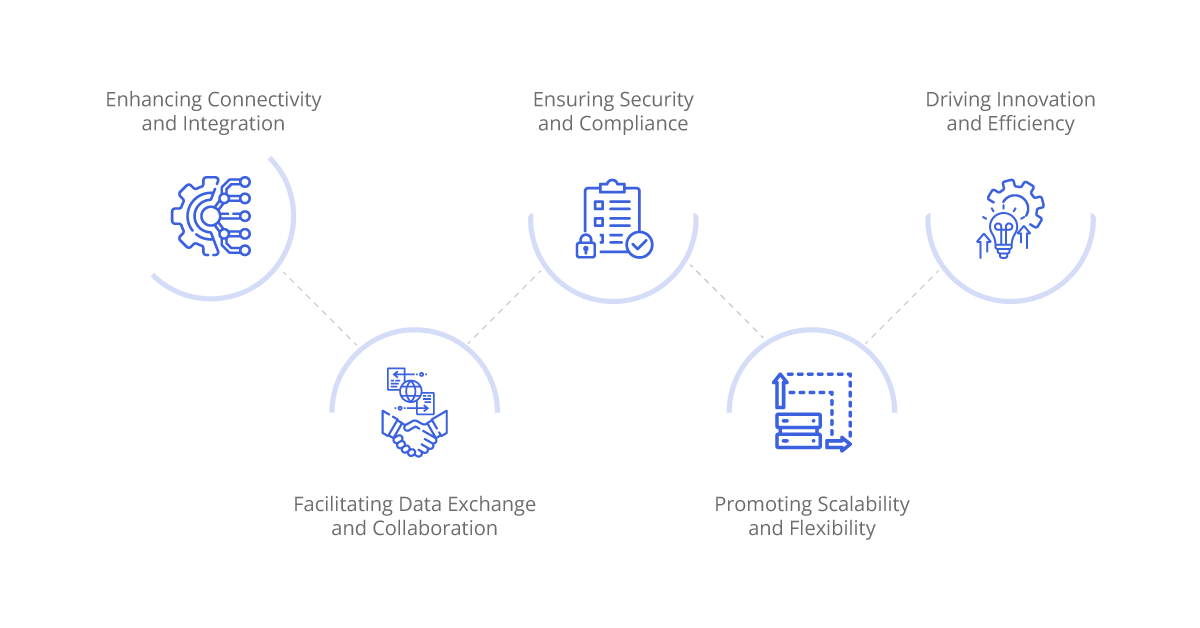
Enhancing Connectivity and Integration
iPaaS serves as a centralized platform that enables healthcare systems to connect and integrate various data sources, applications, and devices. By providing pre-built connectors and APIs, iPaaS simplifies the process of integrating electronic health records (EHRs), laboratory systems, billing platforms, and other critical healthcare applications. This seamless connectivity ensures that essential patient data is readily accessible to healthcare providers, regardless of the system or application used.
Facilitating Data Exchange and Collaboration
With iPaaS, healthcare organizations can overcome the barriers posed by data silos and disparate systems. By standardizing data formats and protocols, iPaaS enables efficient data exchange and collaboration between different departments, healthcare facilities, and external partners. This fosters improved care coordination, enhances communication among healthcare providers, and ultimately, leads to better patient outcomes.
Ensuring Security and Compliance
Security and compliance are paramount in healthcare, and iPaaS solutions like Aonflow are designed with robust security features to safeguard sensitive patient information. Built-in encryption, access controls, and compliance monitoring capabilities ensure that data remains protected and meets regulatory requirements such as HIPAA and GDPR. Additionally, iPaaS solutions offer audit trails and reporting functionalities to provide transparency and accountability in data exchange processes.
Promoting Scalability and Flexibility
One of the key advantages of iPaaS is its scalability and flexibility. As healthcare organizations grow and evolve, iPaaS solutions can easily scale to accommodate increased data volumes, additional applications, and changing business requirements. Cloud-based iPaaS offerings provide the flexibility to adapt to evolving technological trends and integrate new healthcare innovations seamlessly.
Driving Innovation and Efficiency
By leveraging iPaaS for interoperability, healthcare organizations can drive innovation and efficiency throughout their operations. iPaaS enables rapid deployment of new applications and services, accelerates time-to-market for digital health initiatives, and supports agile development methodologies. This fosters a culture of innovation within healthcare organizations and enables them to stay at the forefront of healthcare technology advancements.
Wrapping it Up
iPaaS plays a vital role in enabling interoperability within healthcare systems by facilitating seamless data exchange, enhancing collaboration, ensuring security and compliance, promoting scalability and flexibility, and driving innovation and efficiency. As healthcare organizations continue to prioritize interoperability initiatives, iPaaS will remain a fundamental technology solution for achieving their interoperability goals and delivering high-quality patient care.
Aonflow iPaaS – Free for First 3 Months!
Build and run up to 1,500 transactions monthly with no cost. No payment info needed!